0512-67998889(Suzhou)
18051093220(Shenzhen)
Chimeric Antigen Receptor Macrophages (CAR-M) have demonstrated significant clinical potential in the field of solid tumor treatment due to their superior immune infiltration capabilities and efficient targeted killing efficacy. To further promote the clinical translation and application of CAR-M therapies, it is particularly important to develop a high-efficiency and precise evaluation system to rapidly quantify their infiltration and killing performance. This not only helps to deepen the understanding of the mechanisms of action of CAR-M but also provides solid data support for optimizing treatment plans and improving patient prognosis. Organoid technology, by reducing animal experiments and utilizing human-derived tissues, avoids biases brought about by species differences, making it particularly suitable for patient-specific tumor research and the exploration of infectious disease mechanisms. Additionally, organoids can construct multi-organ systems and be cultured long-term, offering unique advantages for studying the interactions between drugs in multiple organs and their long-term toxic effects. Recently, a joint effort by the RocRock Biotech team, the Puheng Biomai team, and Professor Zhang's team, using Puheng Biomai's self-developed 3D NAC-Organ organoid technology platform, has established a high-throughput in vitro screening system suitable for the HER2-targeting CAR-M cells designed and developed by RocRock Biotech. The latest research results of the scientific team, titled "3D DNA Origami Assembled Spheroid for Evaluating Cytotoxicity and Infiltration of Chimeric Antigen Receptor Macrophage (CAR-M)," have been published in the internationally renowned academic journal Communications Biology. RocRock Biotech is the corresponding author of the paper, with its founder Professor Yin Xiushan, Puheng Biomai founder Dr. Song Guangqi, co-founder Professor Zhao Yicheng, and Professor Zhang serving as co-corresponding authors.
The research team designed and constructed a CAR gene cassette targeting HER2. Using a viral vector with high gene transduction efficiency, the CAR-HER2 gene was introduced into human monocyte-derived macrophages (hMDM) and a mouse macrophage cell line (RAW264.7), achieving more than 85% CAR-positive expression. The study showed that both hMDM CAR cells and RAW CAR cells, despite certain phenotypic differences, exhibited pro-inflammatory phenotypes. This characteristic is beneficial for enhancing the activity of HER2 CAR-M cells in the tumor microenvironment, thereby improving their killing efficiency against tumor cells.
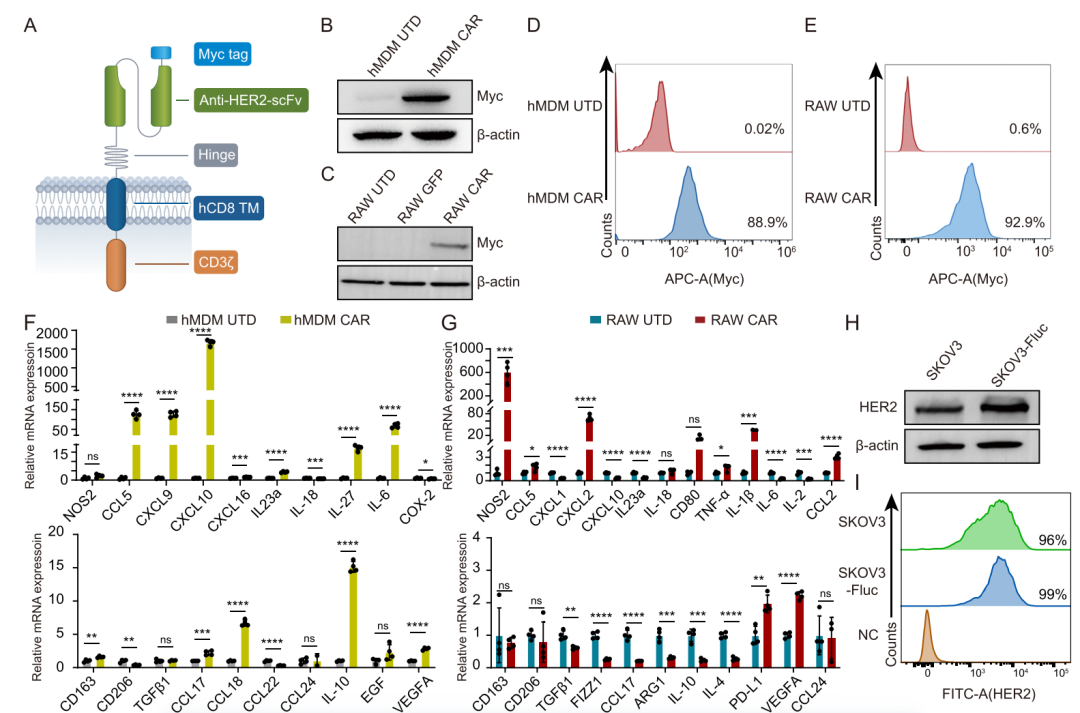
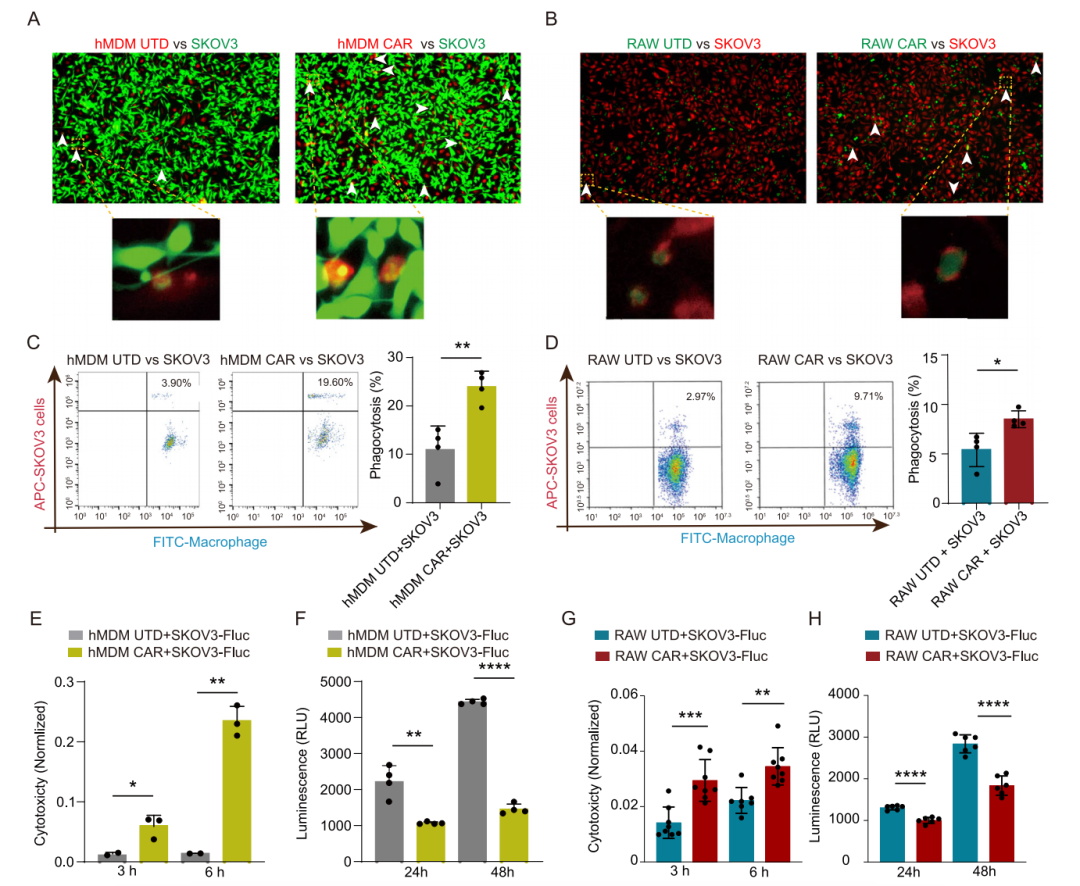
To assess the phagocytic and cytotoxic capabilities of HER2 CAR-M cells against HER2-positive cells, this study selected the ovarian cancer cell line SKOV3, which highly expresses HER2, and SKOV3-fluc, which is labeled with firefly luciferase, as targets. A dual-color labeling strategy was used to stain the CAR-M cells and target cells separately, and the phagocytic efficiency of the CAR-M cells was evaluated after co-culturing. Flow cytometry experimental results showed that the phagocytic efficiency of the CAR-M cell group, including both hMDM CAR cells and RAW CAR cells, was significantly higher than that of the control group for SKOV3 cells. Furthermore, the cytotoxicity of HER2 CAR-M was evaluated using LDH release assays and firefly luciferase activity detection. The former quantifies cytotoxicity based on the detection of LDH enzyme activity released by damaged cells, while the latter reflects changes in cell survival status by monitoring the decrease in luciferase activity. The results consistently indicated that the cytotoxic effect of HER2 CAR-M cells on SKOV3-Fluc cells was significantly enhanced.
The research team utilized their independently developed NAC-Organ technology to construct a 3D ovarian cancer solid tumor spheroid (NAC-Solid Tumor) based on SKOV3 cells. This model possesses high stability and activity, and it does not require matrix gel support, allowing for long-term co-culturing with immune cells, which enables immune cells to actively infiltrate the tumor model. Observations made through a live cell imaging system have shown that macrophages can effectively penetrate this tumor model. This three-dimensional tumor model successfully simulates the dynamic interactions between tumor and immune cells, serving as a robust platform for evaluating the targeted infiltration and cytotoxic efficacy of CAR-M cells.
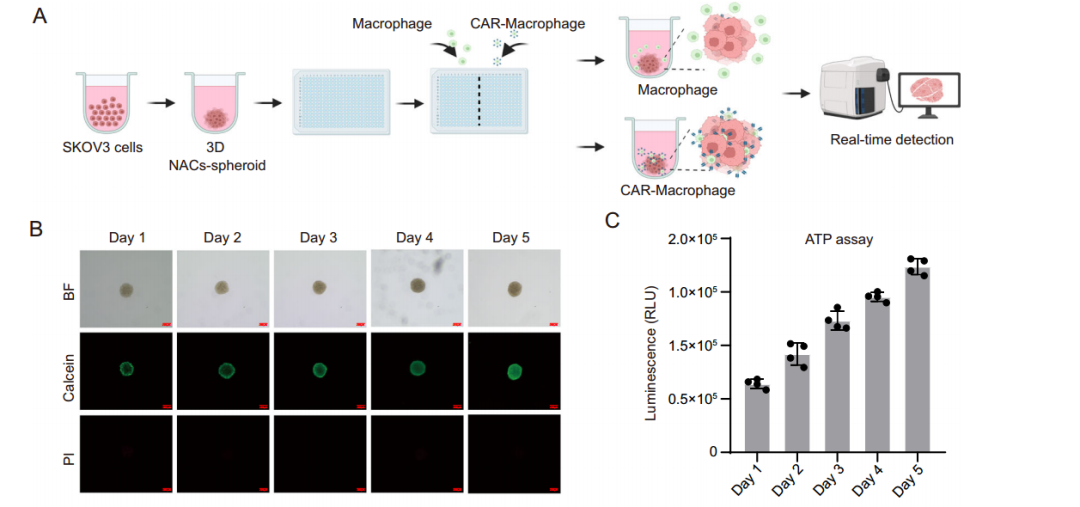
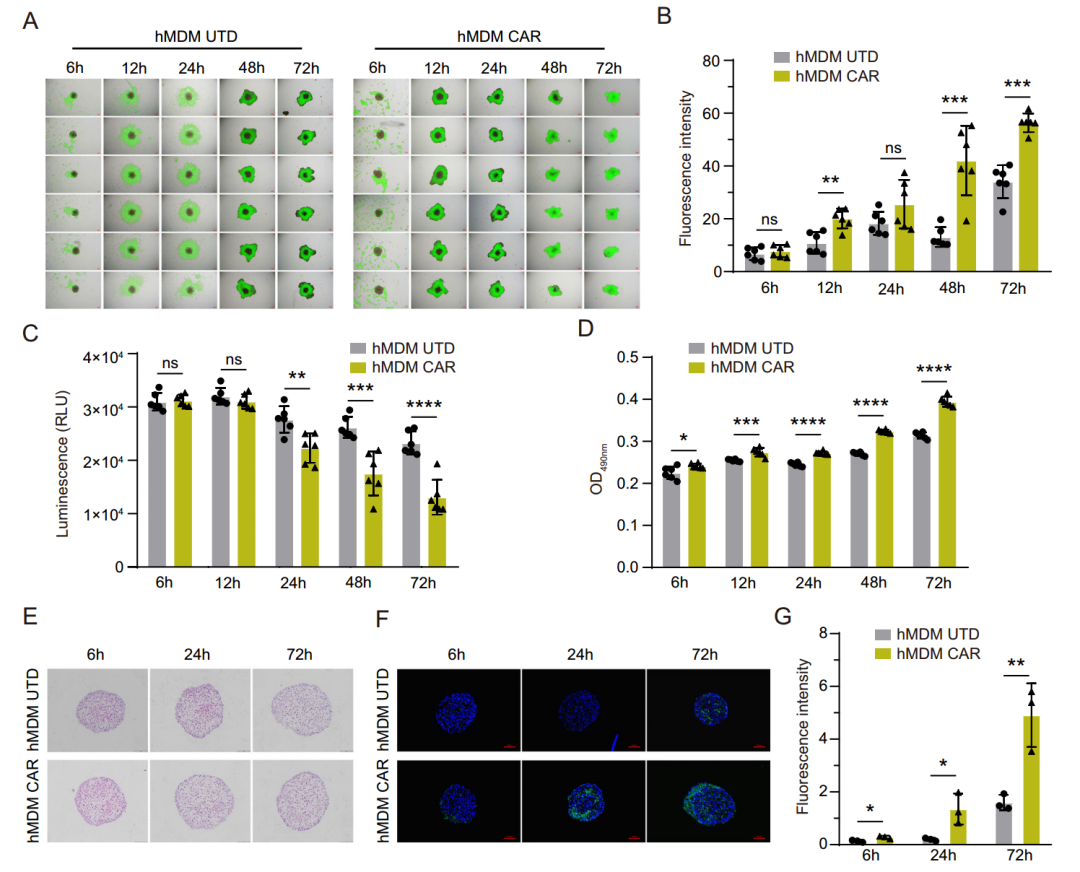
To validate the recognition, penetration, and cytotoxicity of HER2 CAR-M cells against solid tumors, the team constructed a three-dimensional tumor spheroid model using ovarian cancer SKOV3-Fluc cells. By co-culturing UTD-M cells and HER2 CAR-M cells with the tumor spheroids, they assessed the infiltration and cytotoxic effects at different effector-to-target cell ratios (E/T) and incubation times. The results showed that HER2 CAR-M cells effectively infiltrated the tumor spheroids at various E/T ratios, with the most significant effect observed at an E/T ratio of 10:1. In contrast, UTD-M cells exhibited minimal targeting and found it difficult to penetrate deeply into the tumor spheroids. At an E/T ratio of 10:1, the cytotoxicity of CAR-HER2-M cells against the solid tumor spheroids was significantly higher than that of UTD-M cells, and this enhancement in infiltration ability and cytotoxicity gradually increased over time.
This study, by integrating NAC-Organ technology with CAR-M cell therapy, systematically evaluated the targeted infiltration and cytotoxic capabilities of CAR-M cells against solid tumors in a 3D ovarian cancer model, proposing an innovative solution to address the complex challenges of solid tumor treatment. The findings not only lay a solid scientific foundation for the clinical application of CAR-M cells but also provide new ideas and methods for personalized medicine and precision therapy
0512-67998889(Suzhou)
18051093220(Shenzhen)

Cathy.Lv@rocrockbio.com(Suzhou)
lliangjing@rocrockbio.com (Shenzhen)